Introduction
“Woman accused of attacking snoring husband” reports the Washington Post on 18 June 2005. Fifteen percent of the local population snore to varying degrees during their sleep. The overwhelming majority are men and many long suffering wives stay silent. Studies have shown that bed partners of heavy snorers suffer disturb sleep, morning headaches and daytime sleepiness (1). These symptoms improve when the snoring partner receives treatment (2).
How is Snoring Generated?
The sound generated during snoring is caused by the vibration and striking of tissues in the collapsible part of the throat which include the tongue, back wall of the throat, the uvula and soft palate. The level of snoring depends on how hard these tissues strike each other.
Who is susceptible to snoring?
Certain features found in patients make them more likely to snore. These include
- narrow upper airways caused by nasal allergies (causing large turbinates), large tonsils and adenoids (especially in children), large tongue bases.
- poor muscle tone in the throat. Alcohol and certain medications cause reduction in muscle tone allowing the walls of the throat to collapse inwards. This is especially prominent during sleep.
Is Snoring common?
The prevalence of snoring varies from 37% to 87% in adults and 20% to 28% in children.
So what if you are a snorer?
Simple or Habitual snoring (without obstructive sleep apnea, see under OSA) is generally more of a social problem. The snorer is oblivious to the problem until their suffering partner insist getting a medical opinion to solve the problem. 15% of husbands and 50% of wives are bothered by their spouses’ snoring.
When does simple or habitual snoring become Obstructive Sleep Apnea?
It is acceptable and normal for people to have periods when breathing stops during sleep. When each period last more than 10 seconds, it is considered an apneic spell. When someone had more than 5 apneic spells per hour of sleep, that person has Obstructive Sleep Apnea (OSA). Patients can have mild, moderate or severe OSA, depending on the number of apneic spells per hour. Many studies have shown that patients with untreated OSA are more likely to suffer hypertension, heart disease and strokes. It has also been shown that patients with OSA are more prone to car accidents.
Symptoms of Obstructive Sleep Apnea
A detailed history is taken from the patient. Symptoms and signs of OSA would include
- Observed Apnea (partner notices patient stops breathing during sleep)
- Choking or gasping spells – patients wake suddenly feeling a sensation of tightness around his neck, or a need to take a deep breath.
- Broken sleep/ Sleep disruption – waking during sleep for no apparent reason
- Feeling unrefreshed on awakening in the morning
- Excessive Daytime Sleepiness
In addition, patients may present with
- Morning headaches
- Bouts of Dizziness (mainly unsteadiness), difficult concentrating at work
- Personality changes including irritability, short temperedness, depression
- Reduced libido (sex drive)
The assessment for OSA will include a full ENT examination and a Polysomnography (Sleep Study). The Sleep Study essentially measures the level of oxygen levels and frequency of sleep disturbances. Besides giving confirmation, it also allows distinguishing mild, moderate and severe forms of the condition.
How can Obstructive Sleep Apnea be diagnosed?
sleep apnea | PolysomnogramThe accepted Gold Standard test in the diagnosis of OSA is a Polysomnogram or Sleep Study. This can be performed in a hospital setting or as a home-based (Figure 1) study. In the past, the study involved many wires and was cumbersome and uncomfortable for the patient. The more recent sleep study devices are more comfortable and patients have found it more acceptable producing more accurate reflection of their sleep quality. When the cause of OSA is obvious eg. large tonsils in adenoids in children, a sleep study may not even be necessary.

How can Obstructive Sleep Apnea be diagnosed?
sleep apnea | PolysomnogramThe accepted Gold Standard test in the diagnosis of OSA is a Polysomnogram or Sleep Study. This can be performed in a hospital setting or as a home-based (Figure 1) study. In the past, the study involved many wires and was cumbersome and uncomfortable for the patient. The more recent sleep study devices are more comfortable and patients have found it more acceptable producing more accurate reflection of their sleep quality. When the cause of OSA is obvious eg. large tonsils in adenoids in children, a sleep study may not even be necessary.
Other alternatives
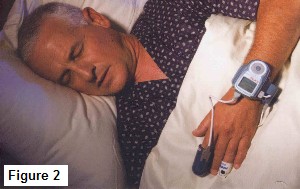
1. Watchpat 200 – this is an upgrade from the Watchpat 100 and is a device that is worn on the arm and measures peripheral arterial tone (figure 2). The advantage lies in its comfort during sleep and has been shown to be accurate when compared with hospital-based sleep studies. The Watchpat 200 offers a comfortable, accurate and convenient way of assessing a patient’s risk for OSA and is the current preferred choice of assessment.
2. Apneagraph – this is an ambulatory device that is designed to measure and localize the level of obstruction in patients with OSA. It combines a sleep study with nasal-pharyngeal pressure measurements to identify the site of obstruction in patients with OSA. The study involves the insertion of a pressure-transducer catheter through the nose into the esophagus. Some patients will find the presence of the catheter running from the nose into the esophagus uncomfortable. There is also a lack of validation of this tool in the medical literature.
Other alternatives
1. Watchpat 200 – this is an upgrade from the Watchpat 100 and is a device that is worn on the arm and measures peripheral arterial tone (figure 2). The advantage lies in its comfort during sleep and has been shown to be accurate when compared with hospital-based sleep studies. The Watchpat 200 offers a comfortable, accurate and convenient way of assessing a patient’s risk for OSA and is the current preferred choice of assessment.
2. Apneagraph – this is an ambulatory device that is designed to measure and localize the level of obstruction in patients with OSA. It combines a sleep study with nasal-pharyngeal pressure measurements to identify the site of obstruction in patients with OSA. The study involves the insertion of a pressure-transducer catheter through the nose into the esophagus. Some patients will find the presence of the catheter running from the nose into the esophagus uncomfortable. There is also a lack of validation of this tool in the medical literature.
Conservative methods include
1. Weight management
In the latest recommendations from the Ministry of Health Guidelines, men should have a Body Mass Index (BMI) from 19 to 23, women from 18 to 22. The BMI can be calculated by dividing your mass in kilograms(kg) by your height in metres twice. For example, a 80 kg man with a height of 1.8m has a BMI of 80/ (1.8×1.8) = 24.7. Patients with BMI over 30 are considered grossly obese. Reduced dietary intake and medications that reduce the absorption of dietary fat can help obtain the ideal BMI.
2. Allergy and Sinusitis Management
Nasal allergies and chronic sinusitis result in swollen nasal lining. This reduces nasal patency and promotes mouth breathing during sleep. The first course in allergy management is conservative with nasal steroid sprays and antihistamines. Surgery is only indicated if conservative methods fail.
3. Oral Appliances
These are worn during sleep. Its principle is to push the lower jaw forward and widen the space in the throat. A common complaint is jaw discomfort although this improves over time.
4. Nasal Continuous Positive Airway Pressure (nCPAP)
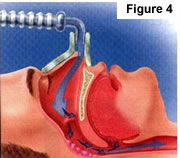
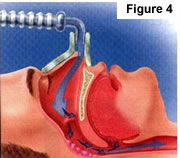
This treatment entails a use of a machine that generates a positive pressure which is transferred to the patient via a mask that covers the nose (figure 3). Instead of having to suck air in (thus causing collapse of the upper airway), the positive pressure pushes air into the lungs while preventing the walls of the upper airway from collapsing (figure 4). The machine is portable and silent. Some patients complain of discomfort while wearing the mask to sleep. In some patients (usually with severe OSA), the positive pressure required to keep the airway patent is so high that air can leak around the mask, reducing the effectiveness of this treatment.

4. Nasal Continuous Positive Airway Pressure (nCPAP)
This treatment entails a use of a machine that generates a positive pressure which is transferred to the patient via a mask that covers the nose (figure 3). Instead of having to suck air in (thus causing collapse of the upper airway), the positive pressure pushes air into the lungs while preventing the walls of the upper airway from collapsing (figure 4). The machine is portable and silent. Some patients complain of discomfort while wearing the mask to sleep. In some patients (usually with severe OSA), the positive pressure required to keep the airway patent is so high that air can leak around the mask, reducing the effectiveness of this treatment.
Apneagraph – this is an ambulatory device that is designed to measure and localize the level of obstruction in patients with OSA. It combines a sleep study with nasal-pharyngeal pressure measurements to identify the site of obstruction in patients with OSA. The study involves the insertion of a pressure-transducer catheter through the nose into the esophagus. Some patients will find the presence of the catheter running from the nose into the esophagus uncomfortable. There is also a lack of validation of this tool in the medical literature.
Apneagraph – this is an ambulatory device that is designed to measure and localize the level of obstruction in patients with OSA. It combines a sleep study with nasal-pharyngeal pressure measurements to identify the site of obstruction in patients with OSA. The study involves the insertion of a pressure-transducer catheter through the nose into the esophagus. Some patients will find the presence of the catheter running from the nose into the esophagus uncomfortable. There is also a lack of validation of this tool in the medical literature.
5. Avoiding Sedatives and Alcohol
Certain medications (including those with drowsiness as a side effect) and alcohol can aggravate snoring and OSA as the walls of the throat become more relaxed and narrow the airway.
Surgical methods include
1. Nasal Surgery
Nasal obstruction resulting from a deviated septum, enlarged turbinates (from allergies), sinusitis and nasal polyps can cause OSA. Up to 30% of patients will notice an improvement in their snoring and sleep quality once their nasal obstruction is relieved. Surgeries to correct the problem include
- Septoplasty (for deviated nasal septums) – one side of the nose can be blocked because the center partition (septum) is crooked. Correcting this deformity will allow more equal and smoother flow of air during sleep.
- Radiofrequency Turbinate reduction (RTR) – the most common cause of nasal obstruction is swollen turbinates. A simple clinic-based procedure under local anesthesia will correct this problem (see under Commonly Performed Clinic Procedures)
- Endoscopic Sinus Surgery (for nasal polyps and chronic sinusitis) – chronic infection of the sinuses results in swelling of the nasal lining and accumulation of discharge in the nose. When medical therapy has failed, surgery to overcome the infection will improve patency
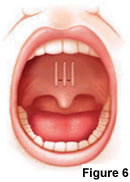
2. Palate Surgery
Much of surgical treatment is aimed at the soft palate. Because of its laxity, the soft palate is responsible for generating much of the sound heard in snoring. Palate surgery is popular because the effects are fairly dramatic in snorers. However, its effectiveness in treating OSA is more controversial.
a. Uvulopalatopharyngoplasty (UPPP) – this procedure is performed under general anaesthesia and involves the removal of tonsils (tonsillectomy) and stiffening of the soft palate.The aim is to widen the palatal opening and to prevent the walls of the throat from collapsing during sleep.

Before surgery – Significant narrowing (arrow) of palatal opening. Little of throat seen from nose
After Uvulopharyngoplatoplasty – notice the significant widening of the palatal opening (white arrow). The larynx (black arrow) is also now seen
a. Uvulopalatopharyngoplasty (UPPP) – this procedure is performed under general anaesthesia and involves the removal of tonsils (tonsillectomy) and stiffening of the soft palate.The aim is to widen the palatal opening and to prevent the walls of the throat from collapsing during sleep.
- Laser Assisted Uvulopalatoplasty (LAUP) – the principle of this procedure (as in all palate surgery) is to cause a certain degree of scarring and hence stiffening of the soft palate, thus reducing its laxity and ability to generate sound. It entails the application of the LASER to the soft palate and uvula under general anaesthesia.
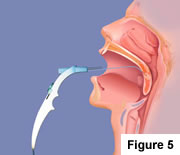
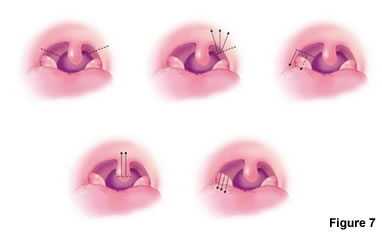
- Radiofrequency (RF) treatment to the soft palate (figure 5) – this is an office-based procedure, performed under local anaesthesia. It may require 2 or 3 applications before results are seen.
- Laser Assisted Uvulopalatoplasty (LAUP) – the principle of this procedure (as in all palate surgery) is to cause a certain degree of scarring and hence stiffening of the soft palate, thus reducing its laxity and ability to generate sound. It entails the application of the LASER to the soft palate and uvula under general anaesthesia.
- Radiofrequency (RF) treatment to the soft palate (figure 5) – this is an office-based procedure, performed under local anaesthesia. It may require 2 or 3 applications before results are seen.
3. Tongue Base Surgery
In certain patients, the bulk of the tongue base is the cause of the obstruction during sleep. Surgery is aimed at pulling the tongue base forward (Geniohyoid advancement, Repose Suspension Suture) or shrinking the tongue base with radiofrequency (Figure 8) can improve the situation. All procedures involving the tongue base are associated with the risk of airway compromise in the immediate post-operative period. Patients require close monitoring and overnight stay in hospital.
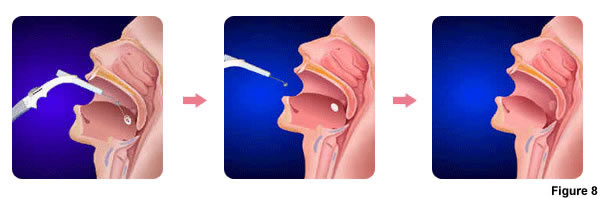
Figure 8 – Sequence of action from left to right. Application of radiofrequency, scarring of tongue tissue, reduction of tongue mass and widening of airway
3. Tongue Base Surgery
In certain patients, the bulk of the tongue base is the cause of the obstruction during sleep. Surgery is aimed at pulling the tongue base forward (Geniohyoid advancement, Repose Suspension Suture) or shrinking the tongue base with radiofrequency (Figure 8) can improve the situation. All procedures involving the tongue base are associated with the risk of airway compromise in the immediate post-operative period. Patients require close monitoring and overnight stay in hospital.
4. Tracheostomy
This surgery is the surest way of making a patient with OSA safe. The procedure involves making a hole in the trachea bypassing any obstruction in the upper airway. Unfortunately, this leaves the patient with an unsightly scar (and hole) and can affect the voice. A tracheostomy generally serves as a last resort in patients who have failed conservative and surgical methods.
Pitfalls in the Management of Obstructive Sleep Apnea
The diagnosis and management of snoring and obstructive sleep apnea (OSA) can be confusing and difficult to understand for a few reasons. The diagnosis of OSA depends on a few factors, not a single parameter. Reading a sleep study is not simple and the cause of OSA is usually multiple and not a single problem. For example, a patient could suffer from OSA because his/her nose is blocked, have big tonsils and is overweight. Treatment has to address all these conditions and treatment options can overwhelm even the most educated patient. Please click on these links to learn more about how to avoid pitfalls in managing OSA.
Case 1 – Overtreatment by ‘Internationally Renowned’ Sleep Surgeon
Case 2 – Medical Insurance Fraud by ‘Internationally Renowned’ Sleep Surgeon
Case 3 – Blatant Attempt by ‘Internationally Renowned’ Sleep Surgeon to Deceive Medical Insurers
